But a disturbing number of news reports have surfaced detailing unlicensed providers injecting all kinds of life-threatening stuff—from industrial silicone to lamb fat—with the goal of Kardashianizing women on the cheap. The FDA issued a safety alert late last year warning the public of the catastrophic risks involved with liquid silicone injections in particular.
All over the country, “people are dying from these shots,” said Beverly Hills liposuction surgeon Aaron Rollins, echoing statements in the FDA alert. Silicone, a permanent synthetic substance, is not FDA-approved for cosmetic purposes, but since it was greenlighted in the 1990s for certain uses in ophthalmology (serious stuff, like retinal detachment), injecting it into the skin to plump and fill lips, breasts, and butts is technically considered “off-label”—i.e. not illegal.
Still, the insidious goo is an infamous troublemaker. “I wouldn’t touch it with a ten-foot pole,” adds Rollins. “It may look good at first, but over time, the body forms scar tissue around it, so the injected area keeps growing and growing, as the silicone weaves its way into your tissues, becoming lumpy and hard, and nearly impossible to remove.”
Subtract an experienced injector from the equation, and silicone goes from dicey to deadly. “You hear about these so-called pumping parties at hotels, where unlicensed doctors visiting from other countries are injecting patients with massive doses of silicone,” says Dr. Clyde Ishii, president of the American Society for Aesthetic Plastic Surgery (ASAPS). “They’re literally buying it from Home Depot or Lowe’s,” he explains, “because it’s so much cheaper and easier to get than medical-grade silicone.” To lower their cost even more, some of these unlicensed doctors mix in toxic filler-type materials, like cement and motor oil, says Miami dermatologist Manjula Jegasothy. “Even in Beverly Hills,” notes Rollins, “there are people using caulk guns to inject stuff into women’s bodies, and tragic things are happening.”
It’s not uncommon for these unlicensed practitioners—inexperienced with human anatomy—to inadvertently shoot silicone into a blood vessel. And when they do, it can travel to the heart or lungs, blocking blood flow, and causing sudden heart attacks and strokes. The risk is especially high when injecting the vascular buttocks. Yet, for some, silicone’s price tag is just too good to pass up. According to Atlanta plastic surgeon Wright Jones, “Silicone butt injections may cost a tenth of the price of a legal gluteal enhancement using one’s own fat”—which is currently regarded as the most effective way to boost a backside. A Brazilian Butt Lift, using liposuction and fat transfer, can cost upwards of $10,000.
In light of the recent wave of silicone horror stories, and with butt augmentation fast becoming one of the most popular plastic surgery procedures in the U.S., not to mention a burgeoning business for untrained injectors, the Aesthetic Surgery Education and Research Foundation (a division of ASAPS) felt compelled to publish a safety protocol for gluteal fat grafting in the current issue of the Aesthetic Surgery Journal.
That’s not to say fat is the only safe solution for a shapeless bottom. Many dermatologists and surgeons do use FDA-approved cosmetic fillers “off-label” here— to either produce an immediate, yet temporary, lift from hyaluronic acid gels; or a gradual, long-term improvement from the collagen-stimulating Sculptra (which is currently only approved to soften the appearance of nasolabial folds). But such shots can be wildly expensive.
Which brings us back to silicone and its unfortunate recipients, many of whom are millennials, says Jones. At age 22, Heather*, a model in Los Angeles, visited a Koreatown medical spa for silicone butt injections. “I was booked to do a big photo shoot, and wanted my bum to look perkier,” she says.
About six months later, she noticed several golf ball-size lumps in her bottom, a common side effect of silicone. On the advice of a trusted friend, Heather says she went to see Rollins, who was able to camouflage the hills and valleys by liposuctioning fat from her arms and injecting it into her butt—an $8,000 fix.
Lips have long been another hot spot for silicone. Tired of having to draw on a juicer pout each morning, Madeline paid $50 to have her lips injected with silicone in a salon basement in Queens when she was 26 years old. Now 40, she says, “I feel like I messed up my mouth for the rest of my life.”
The size and shape of her lips change daily, often with the weather. “Usually in summer [the silicone] lays okay, but in the colder months, it moves around a lot, and concentrates in one area, bulging out.” To have her smile repaired will cost roughly $10,000, she’s been told, and surgeons can’t promise a total improvement.
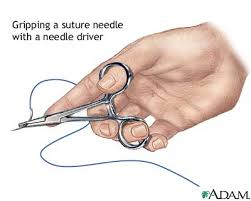
Cosmetic injections should only be performed by board-certified dermatologists or plastic surgeons. If your injector is not, ask thorough questions about their training and experience. How many years have they been injecting patients? What formula are they using? If you’ve found the injector through a bargain website or coupon—the deal is likely too good to be true. The bottom line: Heed the warnings. “Don’t allow silicone into your body—ever,” says Rollins. At best, “you’ll be buying a problem for the rest of your life.”
Now a word from Dr. Sowder: The above article is very well written and is not, I repeat, is not alarmist. People are dying from these injections and others are being maimed for life. I have taken care of a couple of ladies who had silicone injected into their breasts in Asia and cleaning this up is such a mess. Whenever I hear about another silicone injection disaster, usually done by a non-physician in some hotel room, I just shake my head. I mean, really, how dumb can you be? I do not endorse blaming the victim but in cases like this I think the person allowing a charlatan to inject their butt or breast with silicone bears some responsibility. Those on the other end of the calking gun need to go to jail and many in fact have. The lesson here is that you get what you pay for.
Kudos to Ms. Edgar for a cautionary tale and to Harper’s for publishing it. Thanks for reading and don’t let anyone get near you butt or breast with a calking gun! Dr. Lisa Lynn Sowder









 @lisalynnsowder
@lisalynnsowder
