I saw a patient recently who would benefit a lot from having a breast lift at the time of implant removal and that was what I recommended. She had read on Dr. Facebook that it was safer to delay the lift. This launched me into a discussion about the blood supply to the breast, which to a layperson, is a pretty arcane topic. I had to reveal myself for the lousy visual artist that I am and draw out a diagram of the blood supply to the breast with and without implants. Later I was able to find a pretty good diagram of the breast with and without an implant and add some red squiggles of my own representing blood vessels.
Let’s walk though it: The unoperated breast has a very rich blood supply with vessels traveling from the chest wall, through the pec and straight into the breast tissue and also blood vessels traveling more superficially, about 1 cm under the skin surface from the periphery of the breast.
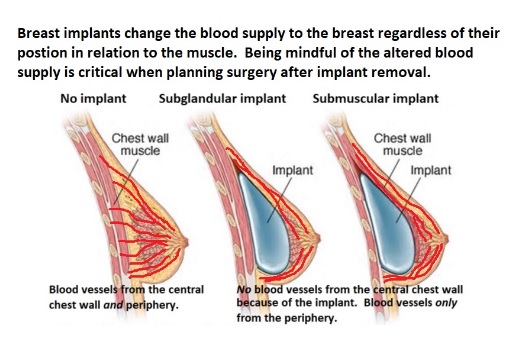
Trouble arises when a surgeon does not recognize the altered blood supply. The most common procedure I do which requires deep appreciation of this altered anatomy is when I do a breast lift following removal of a breast implant. I use a very different technique than I use when doing a lift on a breast that has never had an implant. See this blog for a step by step explanation of a regular breast lift. When an implant has been removed, the peripheral vessels must be preserved or the breast tissue, including the nipple, will lose its blood supply and necrose which is a nice way of saying it will die. When I have just removed an implant, I am on HIGH ALERT in regards to blood supply and also in a position to select the layer of breast tissue that is safe to undermine in order to shape the breast. This sounds creepy but I can place one hand in the implant pocket and the other on the surface of the breast and judge the thickness of the breast tissue and location of the blood vessels. In a delayed case where I wait several months for the breast to heal, I cannot do this because the pocket where the implant had been has disappeared and thus there is no way for me to do the one hand in and one hand on trick. In delayed cases, there will also likely be some scarring and tethering of the tissues that can make safe dissection difficult as well. The very worse case scenario is if a patient who has had implant removed has a lift by surgeon who is not really mindful of this altered anatomy. Using a normal breast lift technique would have a very high risk of tissue necrosis.
so, IMHO, doing a lift at the same time of implant removal has some real advantages. I hope this blog and my fabulous illustration add some clarity. Thanks for reading and I would be honored if you followed me on Instagram @sowdermd and @breastimplantsanity.
Dr. Lisa Lynn Sowder



 @lisalynnsowder
@lisalynnsowder
